Fibrocystic breast disease is a term that may sound alarming, but it actually describes a benign and very common condition that can affect your breast tissue. Nearly half of all women experience fibrocystic changes at some point, so it’s important to understand both the causes and the types. Your breasts are made up of lobules, ducts, and connective tissue; during the menstrual cycle, varying levels of hormones like estrogen and progesterone can influence these tissues, leading to the characteristic lumpy or rope-like textures that are associated with this condition.
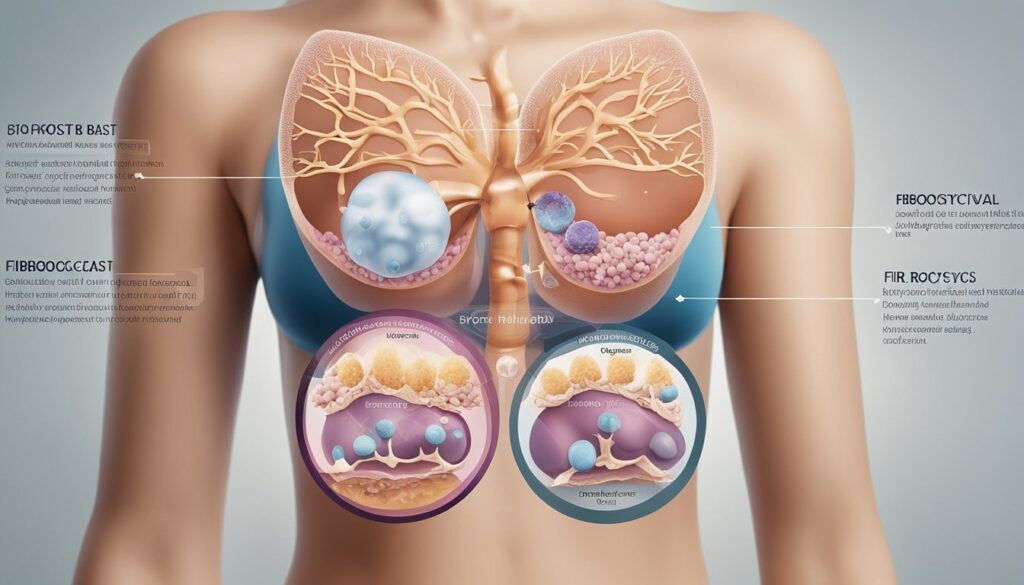
Despite its designation as a disease, fibrocystic breast changes do not increase your risk of breast cancer. The symptoms you might notice, such as breast tenderness, swelling, or the appearance of cysts, are typically most pronounced in the week leading up to your period. This is due to the natural fluctuations in hormone levels, with estrogen causing ductal tissue to enlarge and progesterone leading to a swelling in the lobules. Understanding these patterns can help demystify the experiences you may have with your own body.
Understanding Fibrocystic Breast Changes
Fibrocystic breast changes represent a common and benign condition that often manifests as lumpiness, tenderness, or discomfort in your breast tissue. These changes are typically responsive to your body’s hormonal fluctuations throughout the menstrual cycle.
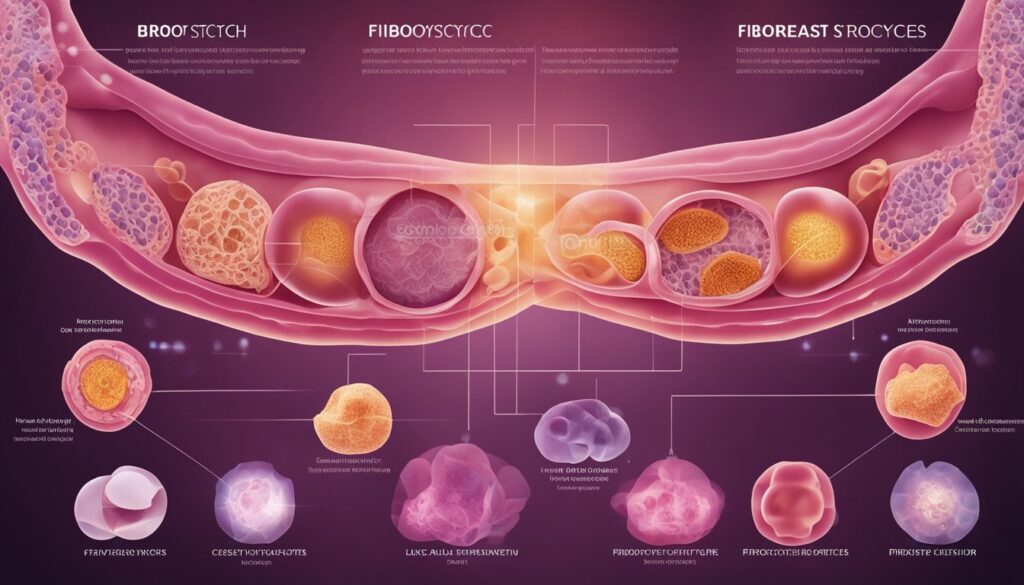
Hormonal Influence on Breast Tissue
Your breasts are particularly sensitive to the reproductive hormones estrogen and progesterone, which are produced by your ovaries. During different phases of your menstrual cycle, levels of these hormones increase and decrease, leading to hormonal changes that can cause breast symptoms. For instance, estrogen’s influence can lead to swelling and fluid retention in breast tissue, while progesterone can cause the glandular breast tissue to enlarge, which is sometimes referred to as adenosis. Collectively, these changes contribute to what you may recognize as mastalgia, or breast pain, particularly in the premenstrual period.
Characteristics of Fibrocystic Breasts
When you experience fibrocystic changes, you may notice a lumpy or ropelike texture in your breasts. These lumps are typically movable and can feel tender or painful, particularly just before your period. They are made up of cysts (fluid-filled sacs) and fibrous tissue, which are considered benign breast disease characteristics. While discomfort due to fibrocystic breasts is common, it’s crucial to monitor the changes. In certain cases, if your discomfort becomes severe or persistent, hormone therapy might be suggested as a treatment option to help alleviate your symptoms.
Diagnosis and Management

In addressing fibrocystic breast disease, it is crucial to accurately diagnose and effectively manage the condition. This involves a blend of clinical examination, imaging techniques, and personalized treatment strategies.
Clinical Evaluation and Imaging
Your healthcare provider will start with a clinical breast exam to assess any palpable breast mass, nipple discharge, or changes like redness or puckering of the skin. They may recommend a mammogram or breast ultrasound if further evaluation is deemed necessary. These imaging tests help distinguish between different types of breast tissue and identify any areas of concern. If a suspicious area is detected during imaging, a biopsy, such as a core needle biopsy, may be performed to rule out malignancy.
Treatment Approaches
The management of fibrocystic breast disease focuses primarily on symptom relief. You may find relief from breast pain and discomfort with over-the-counter pain relievers like acetaminophen or ibuprofen. If you experience more severe symptoms, your doctor might prescribe medications like danazol or tamoxifen. Additionally, certain oral contraceptives can help regulate hormone levels and alleviate fibrocystic changes. Supportive bras can provide physical support, while in rare cases, surgery might be considered. As part of routine care, continue performing breast self-exams and consult your healthcare provider for regular check-ups.
Frequently Asked Questions
In this section, we’ll address some common questions regarding fibrocystic breast disease, helping you understand the variability in types, the impact of diet and vitamins, and the implications of stress and breast symmetry in this condition.
What are the different types of fibrocystic breast conditions?
Fibrocystic breast condition is an umbrella term for a variety of benign breast changes. Typical presentations involve a monthly increase in breast pain or lumpiness that typically improves once your menstrual period starts.
How can dietary changes impact fibrocystic breast disease?
Dietary modifications, particularly reducing caffeine and fat intake, may sometimes alleviate symptoms. It’s advised to maintain a balanced diet rich in fruits, vegetables, and whole grains to potentially ease the symptoms of fibrocystic breasts.
What role does vitamin E play in the management of fibrocystic breast disease, and what is the recommended dosage?
Vitamin E is sometimes suggested for managing tenderness associated with fibrocystic breasts. Although there’s no standard dosage, studies often use amounts ranging from 200 to 600 IU daily, but you should consult with a healthcare provider before starting any supplementation.
How long do fibrocystic breast lumps typically persist?
Fibrocystic breast lumps fluctuate with the menstrual cycle, often becoming more pronounced before menstruation and then diminishing after the period begins. Persistent lumps should be evaluated by a healthcare professional to rule out other conditions.
Is there a correlation between stress levels and the development of fibrocystic breasts?
While there’s no direct causal link established, stress can affect hormone levels, and since fibrocystic breasts are related to hormonal fluctuations, managing stress might help in reducing the symptoms.
Is it common for fibrocystic breast conditions to affect only one breast?
Fibrocystic changes can occur in one or both breasts, but they are often symmetrical. However, it’s possible for one breast to feel more lumpy or painful than the other, and any new or asymmetrical changes should be assessed by a healthcare provider.