Testosterone deficiency, commonly known as low testosterone or Low T, is a medical condition that can affect men, particularly as you age. Your body’s natural production of the hormone testosterone is integral to your growth, development, and overall health. This hormone plays a critical role in your muscle mass, bone density, and sex drive. When levels fall below the normal range, you might notice a variety of symptoms that can impact your quality of life.
Reduced testosterone levels can lead to changes that you might initially attribute to aging, such as fatigue, a decrease in libido, and increased body fat. Beyond these physical symptoms, testosterone deficiency can also affect your mental health, with potential mood swings or a lack of focus. It’s important for you to understand that these changes can be more than just typical signs of getting older; they could be indicative of a hormone imbalance that may require medical attention.
A proper diagnosis of low testosterone requires medical evaluation, often through blood tests that measure your blood testosterone level. If diagnosed, treatment options typically include testosterone replacement therapy, which can be tailored to your individual needs. While this therapy can improve the symptoms and quality of life in those with testosterone deficiency, it’s crucial to be aware of the benefits and risks involved with treatment.
Understanding Testosterone Deficiency

Understanding testosterone deficiency, commonly known as hypogonadism, involves recognizing its impact on your body’s functions, the factors contributing to its onset, and the symptoms it presents. By comprehending these elements, you can better identify and address this hormone-related condition.
Biological Roles of Testosterone
Testosterone plays a crucial role in your body, influencing various physiological processes. Testosterone levels are vital for maintaining:
- Muscle mass and strength
- Bone density
- Facial and body hair growth
- Normal reproductive and sexual function
- Red blood cell production
It’s also associated with your overall energy levels and mood.
Common Causes and Risk Factors
Several factors might lead to low testosterone levels or affect testosterone production, including:
- Aging: Natural decline in hormone levels with age
- Obesity: High body fat can affect hormone production
- Injury: Damage to the testicles can impair testosterone production
- Medical treatments: Chemotherapy or radiation can affect testosterone
- Health conditions: Infections like mumps, HIV/AIDS, Klinefelter syndrome, or issues with the pituitary gland
Understanding these risks can prompt you to monitor symptoms and seek early medical intervention.
Signs and Symptoms
If you experience low testosterone levels, you may notice a variety of symptoms:
- Sexual function: Decreased libido or erectile dysfunction (ED)
- Physical changes: Loss of muscle mass, increased body fat, gynecomastia
- Body and facial hair: Thinning or loss of hair
- Psychological impact: Mood swings, fatigue, depression
- Blood: Anemia or variations in red blood cell count
Being aware of these signs can guide you to seek evaluation and potential treatment for testosterone deficiency. If you notice these symptoms, consider discussing them with your healthcare provider, who can determine if testosterone replacement therapy might be beneficial for you.
Diagnosis and Evaluation
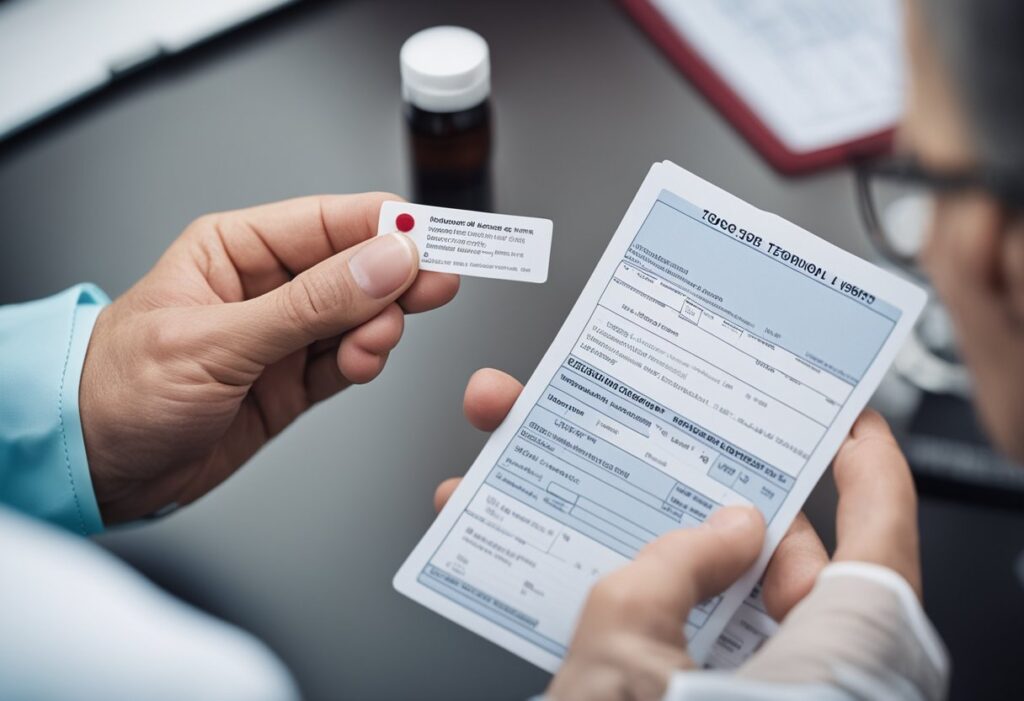
Diagnosing testosterone deficiency involves a careful review of your symptoms, a thorough physical examination, and specific blood tests. It is crucial to evaluate hormonal levels and rule out other medical conditions.
Physical Examination and Medical History
Your doctor will perform a physical exam to check for physical signs of testosterone deficiency, such as reduced body hair, smaller testicles, or gynecomastia (enlargement of the breasts). A detailed medical history can reveal symptoms related to testosterone deficiency, including fatigue, low libido, and difficulty concentrating. Understanding your health history helps in identifying any potential causes of testosterone imbalance, such as pituitary disorders or injuries to the testes.
Blood Tests and Hormonal Evaluation
Blood tests are essential in confirming low testosterone levels. Your doctor will look for a testosterone level below 300 nanograms per deciliter as an indicator of testosterone deficiency. It’s important to measure luteinizing hormone (LH), as elevated levels can signal a primary testicular failure. If a pituitary tumor is suspected, other hormone levels, including prolactin, may be assessed.
- Total Testosterone: Normal range varies, but it’s often considered low if < 300 ng/dL.
- Free Testosterone: May be measured if total testosterone is borderline low.
- LH: Can indicate primary or secondary testosterone deficiency.
Repeated blood tests may be needed to confirm low testosterone levels because of fluctuations throughout the day.
Additional Diagnostic Procedures
Further diagnostic tests may be warranted based on the results of your physical examination and initial blood tests. The evaluation of your pituitary gland function, thyroid health, and potential issues with fertility could include:
- Semen Analysis: To assess sperm count and sperm production.
- Bone Density Test: To check for bone health, which can be affected by testosterone levels.
- Pituitary Imaging: MRI scans to identify pituitary tumors or abnormalities.
In cases of delayed puberty or suspected genetic conditions, additional tests may be conducted to explore these possibilities.
Treatment Options and Management
When addressing Testosterone Deficiency, your management plan can involve making lifestyle changes, undergoing Testosterone Replacement Therapy, and considering various medications and supplements. Each of these interventions can help mitigate symptoms and improve your quality of life.
Lifestyle Changes and Health Optimization
Lifestyle adjustments can play a significant role in managing low testosterone levels. Achieving a healthy weight and engaging in regular physical activity can improve your sex drive, mood, and bone mass. It’s essential to reduce stress, as it can exacerbate symptoms. A nutritious diet and adequate sleep can also support hormonal balance and overall health. Be mindful that some lifestyle changes can also help mitigate the risk of sleep apnea, a condition commonly associated with low testosterone.
Testosterone Replacement Therapy
Testosterone Replacement Therapy (TRT) is a widely used treatment involving the administration of testosterone through injections, gels, patches, or pellets. This therapy can lead to an improvement in various symptoms like low sex drive, decreased energy levels, and loss of muscle mass. However, TRT comes with potential side effects and risks including an elevated risk of blood clots. It is critical to discuss these risks with your healthcare provider and undergo consistent monitoring to maintain therapeutic testosterone levels. More information on TRT protocols can be found at the Cleveland Clinic.
Medications and Supplements
Besides TRT, other medications could be prescribed to address specific causes of Testosterone Deficiency. Certain hormonal medications help stimulate testosterone production. A healthcare professional may also recommend supplements that support overall hormone health. However, the efficacy of supplements can vary, and they should only be taken under the guidance of a healthcare provider. For patients undergoing TRT, American Urological Association guidelines suggest monitoring to ensure optimal treatment and management of symptoms.
Long-Term Considerations and Monitoring
Effective management of testosterone deficiency involves not just initiating treatment but also ensuring ongoing monitoring and addressing potential long-term health implications. Your treatment journey is tailored to mitigate risks and promote overall health.
Monitoring and Ongoing Care
Your testosterone therapy requires regular follow-up to assess its effectiveness and adjust dosing as necessary. Blood tests to monitor your testosterone levels, hematocrit to check for increased red blood cells, and lipid profiles for heart health are vital. You’ll typically undergo these tests every 3 to 6 months or as directed by your healthcare provider.
- Testosterone Levels: Ensure they are within the therapeutic range.
- Hematocrit: Elevated levels can increase the risk of high blood pressure and other cardiovascular issues.
- Lipid Profile: To monitor cholesterol levels, crucial in managing heart disease risk.
Blood testing helps tailor your treatment, avoiding insufficient or excessive dosing that could lead to unwanted effects such as acne or mood fluctuations.
Potential Complications and Risks
While testosterone therapy can be transformative, you should be aware of possible risks and manage them proactively.
- Cardiovascular Health: Keep an eye on risk factors for heart disease; discuss any concerns with your healthcare provider.
- Prostate Health: Regular prostate screenings are recommended, as there’s a debate about the influence of testosterone on prostate cancer risk.
- Osteoporosis Prevention: Adequate testosterone levels contribute to bone density maintenance, warding off osteoporosis.
- Body Composition: Monitor changes in body fat distribution and muscle mass.
- Emotional Well-being: Be alert for changes in mood or signs of depression.
Additional considerations include monitoring for signs of breast tissue enlargement, hot flashes, or high blood pressure, all of which might require adjustments to your treatment plan. Your healthcare provider will guide you through these checkpoints to maintain optimal health.
Conclusion
Testosterone deficiency (TD) is a medical condition with significant potential impacts on your health and quality of life. Managing TD effectively requires understanding both its symptoms and long-term implications. In cases of TD, you may be at an increased risk for developing osteoporosis, as testosterone plays a pivotal role in bone density maintenance.
Your cardiovascular health can also be influenced by testosterone levels. A deficiency might be a contributing factor to heart disease, making regular screenings and a proactive approach to cardiovascular care highly advisable. While there has been concern about the relationship between testosterone therapy (TST) and prostate cancer, current research indicates that TST is generally safe when monitored properly. However, vigilance and regular prostate screenings remain essential.
TD has links to metabolic disorders such as high blood pressure. If you have TD, managing blood pressure becomes even more critical to minimize additional health risks. It’s important to note that TST has seen an upswing in use, partly due to the increased incidence of testosterone deficiency diagnoses.
Effective management of TD requires a personalized approach, often involving lifestyle adjustments, medication, or hormone replacement therapies. Your healthcare provider can assess the underlying cause of TD and propose a tailored treatment plan. Utilizing treatments that have undergone extensive research will ensure that you are opting for safe and evidence-based options.
Regular follow-ups with your healthcare provider are key, as adjustments to therapy may be necessary. These actions will help maintain your health and enhance your well-being when dealing with testosterone deficiency.
Frequently Asked Questions
This section provides insightful answers to common inquiries regarding Low Testosterone and Testosterone Deficiency.
What are the treatment options for low testosterone in young males?
For young males with low testosterone, treatment options typically include testosterone replacement therapy (TRT) under medical supervision, lifestyle modifications such as exercise and diet, and addressing underlying health conditions that may be affecting testosterone levels.
At what levels is testosterone considered dangerously low?
Testosterone is considered dangerously low when levels fall below 300 nanograms per deciliter (ng/dL). This threshold can signal hypogonadism, necessitating medical evaluation and potentially urgent treatment.
How does testosterone deficiency manifest differently in men and women?
In men, testosterone deficiency may lead to reduced muscle mass, decreased libido, and erectile dysfunction, while in women, it can cause symptoms such as low sex drive, fatigue, and muscle weakness. Women naturally have lower levels of testosterone, which means the symptoms can be subtler and often go unnoticed.
What can be expected if a male has low testosterone levels?
If you have low testosterone levels, you might experience decreased sex drive, erectile dysfunction, reduced muscle mass, increased body fat, and emotional changes like depression or irritability. It’s important to consult a healthcare provider for a proper diagnosis.
What are the common symptoms indicating testosterone deficiency?
Common symptoms indicating testosterone deficiency include low libido, fatigue, muscle weakness, depressed mood, and difficulties with concentration and memory. Men may also experience erectile dysfunction and a decrease in beard and body hair growth.
How can individuals with low testosterone improve their condition?
Individuals with low testosterone can often improve their condition by adopting a healthier lifestyle, including regular physical activity, a nutritious diet, adequate sleep, and stress management. Medical treatments like testosterone replacement therapy also play a critical role when lifestyle changes are insufficient. It’s essential to consult with a healthcare provider for an appropriate treatment plan.